Billions of people around the world have now received a Moderna or BioNTech-Pfizer COVID-19 vaccine. Created with synthetically developed messenger ribonucleic acid (mRNA) that replicates one portion of the virus – its spike protein – the vaccine trains our immune system to recognize and attack SARS-CoV-2 (the virus’s more formal name).
The vaccines, which were developed with unprecedented speed, have proven to be highly effective. Their success heralds a new approach to addressing disease.
“There’s a lot of excitement about RNA therapies,” says biochemistry professor Philippe Gros, PhD’83, McGill’s deputy vice-principal (research and innovation). “If we can design an RNA template to make a vaccine against COVID-19, the same could be done for other diseases. With RNA you can target any protein in the cell.”
Behind the mRNA vaccine’s stunningly successful debut lie decades of research.
“This field has been developing since mRNA was first discovered in 1961. But even 10 years ago, no one thought that mRNA per se could be a drug,” says biochemistry professor Jerry Pelletier, BSc’81, PhD’88.
The journey of discovery has seen some significant contributions from McGill, long recognized as a major player in RNA biomedical research.
The University is home to roughly 100 researchers whose work is focused on RNA science or genomics (you need to know what genes are responsible for what in order to develop effective RNA therapies), and McGill has attracted about $300 million in research funding in the last five years in these areas.
McGill’s ground-breaking RNA research efforts began with biochemistry professor Nahum Sonenberg, who joined the University in 1979 after having already made significant discoveries about how the genetic code from DNA is transmitted through mRNA to instruct ribosomes on what proteins (the fundamental construction materials of organisms) to produce.
Genetic information from DNA is taken by mRNA to direct our cells on how to build our unique bodies: a process known as translation. Over the past 40 years, Sonenberg’s lab has explored what happens when there are errors in translation, revealing how that can lead to a wide range of disorders that include cancer, diabetes, and autism.
“Sonenberg worked out the molecular mechanisms that determine the efficiency of mRNA’s protein output,” says Pelletier, formerly a graduate student with Sonenberg in the 1980s. “He’s the guru at McGill in terms of his contribution to mRNA technology.”
Sonenberg and his team continue to make important discoveries; a 2017 publication demonstrated that pseudo-uridine incorporated into mRNA can not only prevent it from being recognized as a foreign entity by cells – reducing its efficacy as a vaccine – but can also increase translational output.
Displacing a virus
Pelletier’s lab has made its own important discoveries focusing on the translation process and exploring the potential of mRNA for cancer therapies. “With the onset of the pandemic, we started to study the SARS-CoV-2 virus using an old trick in virology, which is to have more than one virus infect the cell.”
The DNA from these viruses is broken up and recombined, a process known as recombination. And as you continuously do this with the virus stock, you see a decrease in viral titers – that is, the lowest concentration of the virus that can still infect a cell.
“Then you re-propagate into a new cell line for a few days, take what comes out, and redo the infections over and over,” Pelletier explains. The result: the majority of the virus’s genome is gone, and you have new, less harmful RNA entities called defective interfering particles (DIPs).
“You can think of DIPs as parasites on the virus, as they maintain the ability to replicate but only in the presence of the original virus – where they replicate at a rate much higher than that virus. If they go into a cell on their own, in the absence of the parental virus, they don’t replicate.”
Thus, if a patient with COVID-19 receives a therapy based on these DIPs, the fast-replicating but harmless DIPs would soon displace the harmful original virus. “So these particles could be used therapeutically to dampen a viral infection, maybe through a nasal spray,” says Pelletier. “We’re now undertaking experiments in mice to see if we can use them to blunt SARS CoV-2 infection.”
The therapeutic potential of mRNA goes beyond vaccines: for instance, it could be used to replace missing or defective proteins or to trigger the immune system so that it can recognize a cancer protein as foreign. And RNA therapeutics goes beyond just mRNA, as there are a number of different types of RNA, each type performing a specific role and offering unique therapeutic possibilities.
For instance, small interfering RNA (siRNA) will activate biochemical reactions that degrade a target RNA molecule, usually mRNA, thus knocking it out. “It’s analogous to having a drug that will inhibit the protein function,” says Pelletier. “You can deliver this siRNA to knock out its target, which could be a viral RNA or a mutated mRNA that’s causing a hereditary disorder. By knocking down the mRNA, you get rid of the faulty protein.”
RNA can also perform a regulatory function, controlling the expression of other genes.

“So, it plays a significant role in disease,” says Gros, whose lab has focused on such infectious diseases as tuberculosis, malaria, and legionella. “What makes some people and not others susceptible to certain infections?”
Genetic sequencing enables researchers like Gros to acquire an individual’s entire genetic profile, which can then be screened for mutations.
“We use single-cell analysis, in which you separate individual cells and sequence each cell’s entire RNA content,” explains Gros. “If you’re studying the immune system, which has a great diversity of cells doing different things, it’s not always easy to understand which cell type is affected in a disease. Single-cell sequencing allows us to look at, say, 50,000 cells from a patient’s blood and compare them to a normal sample to see if something is missing, or not properly activated in response to an infection. And when we find a candidate gene, then we can reconstruct a mouse model to study the human disease.”
From there, the faulty genetic code can conceivably be reprogrammed through RNA approaches. “Even for cancer treatments, there are certain tumors that activate certain pathways and those pathways can be silenced with a whole range of RNA-based methods,” says Gros.
There are other novel ways in which RNA can be applied to address diseases. Take the case of schistosomes, a type of parasitic flatworm released into fresh waters by freshwater snails across Africa, Asia, South America, and, increasingly, Europe.
Once in the water, they can infect humans, where they replicate, affecting the immune system and eventually causing severe organ damage. The World Health Organization has designated schistosomiasis a neglected tropical disease, noting that both acute and chronic schistosomiasis affects primarily poor and rural communities. In 2019, it afflicted 236.6 million people, and about 800 million people are at risk from the condition, ranking it the world’s second most damaging disease, after malaria.

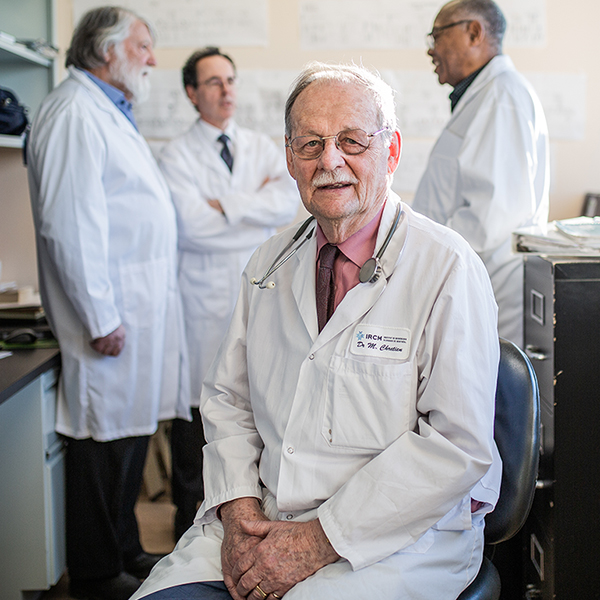
“Those afflicted are primarily women and children, who collect the fresh water,” says Momar Ndao, director of the National Reference Centre for Parasitology and an associate professor in McGill’s Department of Experimental Medicine.
The parasite enters through the skin and works its way to the blood vessels near the intestine or liver.
“We found that the parasite eats while sitting on the vein, because they need to grow,” explains Ndao. “From there, they will migrate to the liver, where they lay eggs.” His research discovered that the parasite needs cathepsin B, a cell enzyme, to grow strong and healthy, so his team has developed a vaccine that uses mRNA technology to block the production of that enzyme.
Tests on mouse models show promising results: the parasite is starved, limiting its reproductive capacity and, by interrupting the life cycle, reducing its potential as a chronic condition. Ndao’s lab is also using RNA technology to address other parasitic infections such as cryptosporidiosis, an intestinal disease that can be life-threatening for immunocompromised individuals.
Partnering with Moderna
Ndao’s research is among the first to take advantage of an agreement McGill entered into with Moderna in March. The company has launched a global initiative, the mRNA Access program, that enables scientists to take advantage of its sophisticated platform to produce candidate vaccines.
McGill was the first Canadian university to sign on with Moderna, which is looking to maximize on their investments by making the platform available to academic researchers. Ndao isn’t the only McGill scientist planning to make use of this new partnership with Moderna. Anne Gatignol, a professor of microbiology and immunology, and of medicine, hopes to use Moderna’s mRNA Access platform to develop a potential vaccine for HIV based on her lab’s work.
The McGill-Moderna partnership is the extension of a deep connection with the company. Noubar Afeyan, BEng’83, one of Moderna’s co-founders, is a McGill graduate, as is Hamilton Bennett, BSc(FSc)’07, the company’s senior director for vaccine access and partnerships.
The Moderna agreement means that McGill researchers, like Ndao, can fast-track their projects by taking advantage of the company’s vaccine-producing technologies. Part of the package involves the company taking a share of the intellectual property, although these agreements are negotiated separately for each project.
In May, Moderna made another announcement, one that should boost Montreal’s status as a research hub for RNA science. The company will build a vaccine production facility in the city that, once it is fully operational, will be able to produce up to 100 million COVID-19 vaccine doses per year.
The press conference was held at McGill, and Prime Minister Justin Trudeau, BA’94, and Premier François Legault both visited some of the University’s genomic and RNA research laboratories before the announcement was officially made.
In an interview with le Journal de Montréal, Moderna CEO Stéphane Bancel said he was looking forward to forging new connections with Montreal researchers in the life sciences sector. “There is a very strong academic fabric in Montreal. We want to open a network that allows for collaboration, particularly with McGill.”
Concerns about equity
While the promise of RNA-based therapies is sparking a research revolution, ensuring that these therapies are equitably accessible and distributed remains an important challenge.

“With COVID-19 mRNA vaccines we’ve seen an unequal rollout across the world for various reasons,” says Amélie Quesnel-Vallée, McGill’s Canada Research Chair in Policies and Health Inequalities and the director of the McGill Observatory on Health and Social Services Reforms.
“One reason is technological: the cold chain required for transporting and storing the vaccines are challenging for countries that are not wealthy.” Further, she notes, vaccines requiring multiple doses inevitably experience attrition – especially among vulnerable populations, who may have more difficulty finding time and means to get to vaccination points.
“If you have to take an appointment and you don’t have medical leave, or you have several jobs, you can’t really take time from work hours to get vaccinated,” says Quesnel-Vallée. “So, considering how to support populations that are in positions of vulnerability can help us deliver better care.”
And, of course, wealthy countries simply bought up most supplies of vaccines, leaving fewer available for less wealthy countries. Quesnel-Vallée stresses that the combination of social science, ethics, and participatory approaches can help address these issues more effectively.
An important factor to consider as we use recent RNA advances to develop new therapies is that, historically, most medical research has been carried out on white males. “And so that left out significant groups: women, people of colour, and other under-represented groups,” says Quesnel-Vallée. “So that concern is at the forefront of having more representative genomes in databases, which would increase the diversity of the genomes used in studies.”
RNA technologies promise a paradigm shift in medical therapies, but time alone will tell how much of this promise can be kept. Currently, though, RNA’s therapeutic potential is vast, as RNA allows researchers to target any protein in the cell without needing pharmacological filters.
Further, because the RNA template already exists, creating a therapy for a specific disease could be as simple a matter as plugging the necessary new genomic information into that template – and by-passing years of laborious experimentation before going to pre-clinical trials.
“As far as many rare diseases are concerned, it’s not too far-fetched to anticipate RNA-based technologies in the near future,” says Gros. “And I don’t mean in 10 years. I mean very quickly.”