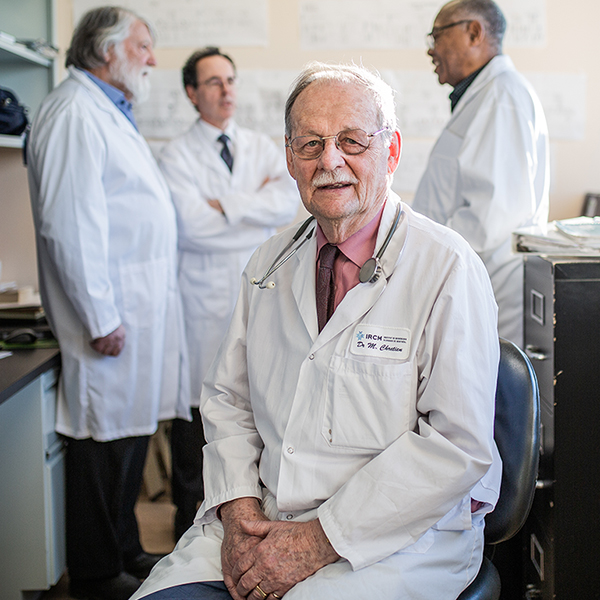
It is difficult to imagine a more dramatic shift for a physician to make than the one Dr. Stefanie Green, MDCM’93, made six years ago.
For the first part of her career, Green’s practice focused on maternal and newborn care and a lot of her time was spent in the maternity ward. Today, she is recognized as a Canadian pioneer in the practice of medical assistance in dying (MAiD).
In 2016, shortly after the federal government passed the legislation that permitted MAiD (with restrictions), Green began offering assisted dying to qualified patients.
She is now the president and co-founder of the Canadian Association of MAiD Assessors and Providers (CAMAP), which has more than 400 members. She is a medical advisor to the B.C. Ministry of Health MAiD oversight committee, and she has provided expert testimony about MAiD to Parliamentary and Senate committees.
Earlier this year, she published This Is Assisted Dying, a book that explores the reasons why some patients seek assisted deaths and how Green has approached her role as a MAiD provider. Publisher’s Weekly described This Is Assisted Dying as “a stunning account” that was “written with sensitivity, grace, and candour.” Green spoke to the McGill News about the book and her work.
You start the book by talking about some of the first patients who reached out to you for MAiD. Why did you decide to start the book that way?
I chose to tell the story of Ed, an amateur clown, in the prologue because his story epitomizes and helps to explain what assisted dying is. It’s a legal and safe procedure and is really meant for individuals. That can mean anyone who qualifies for this care and feels they truly need it, even an eccentric like Ed (who wore a clown suit for the procedure).
I wanted to show a quick example of what the procedure can look like, the individuality of it, and the fact that the subject itself is not necessarily morose. The use of humour and talking about death and dying can help conversation and make this more accessible. Ed’s story encompasses all of that.
When you started this work, did you think of yourself as a pioneer in this field?
I knew I was one of the first clinicians in Canada to step forward and do this work. I was aware of the responsibility of doing it well, and to the highest of standards.
I made a very conscious choice that I wouldn’t do this work behind closed doors. I would do this out in the open, so to speak, like any other kind of medical practice that is legal and paid for. So, I didn’t shy away from talking about what I was doing, speaking to the public about it. I was aware that I was leading the way in that.
As they currently stand, are Canada’s laws up to date with the needs of patients? Do they fall short in some ways?
I won’t comment on that; that will be a debate for the public and officials for many years to come. At CAMAP, we don’t advocate for changes in the law. However, we are able to provide frontline feedback on what’s working and what’s not, the obstacles in the system, and where they might be streamlined.
As a national organization, we at CAMAP are not advocates for assisted dying; we are advocates for those who do the work. We are also a leading voice in setting the highest medical standards for this work, within the framework of the law as it stands at any given time.
In your book, you use the term “reclaiming death and dying.” Can you explain what that means?
It means embracing the fact that death is a natural and inevitable stage of life. We should be talking about it more and preparing for it much earlier. That way, the end-of-life experience is less traumatic and a better experience for all, whether or not it is an assisted death.
Is MAiD an extension of a larger trend, in which patients are consulted at every stage and about every aspect of their treatment options?
Yes. Today, the principle of patient-centred care has replaced the previously more paternalistic system, in which the doctor knows best, and the doctor decides. The rise of MAiD, and the legality of it, is an outcropping of that process, and of respect for the autonomy of the patient.
In the book, you write that MAiD is largely about empowering patients and helping them regain a measure of control.
When I tell someone they are eligible for MAiD, that alone is very therapeutic; I see a remarkable transformation, almost every time. They stop thinking about how they might die and start thinking about how they are going to live during the time they have left.
What is the impact of the pandemic on your work?
It has had an impact on the administration of MAiD. COVID has resulted in restricting the intimacy that is normally involved; huddling around the loved one, holding their hand, saying your final goodbyes. It became a more medicalized event. We are currently working on adjustments to improve on that.
A more positive impact is that the widespread use of telemedicine has meant that remote areas now have greater access to MAiD. We can make a long-distance assessment of a person’s eligibility.
In addition to your duties as president of CAMAP, do you still practice MAiD?
Yes, so that I can better represent the people who do the work; I need to stay in touch and understand the relevant issues, and not just on a theoretical level.
There is another reason. I continue to practice because this is very important and meaningful work. When I help a person facilitate their final wishes, I feel I have done something good. I have given them something that nobody else can, and that is a privilege.